Revenue Cycle Management for a physician practice, healthcare facility, or any other type of insurance-accepting medical entity is predicated upon medical billing and medical coding. The medical billing process and the medical coding process are distinct yet intertwined processes within the revenue cycle to ensure that providers get reimbursed by patients and federal or private insurance payers for the services that they rendered via proper claim submission. It is critical that every healthcare entity optimizes its medical billing and medical coding process in order to receive payment for the delivery of healthcare services.
What is Medical Billing?
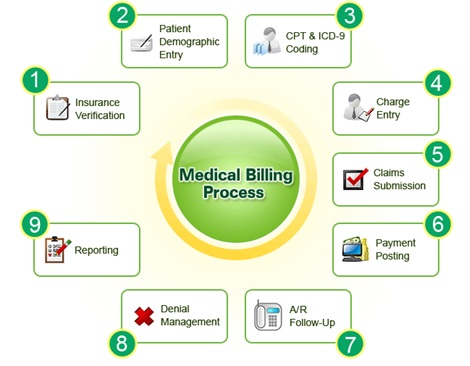
The process for medical billing initiates when a patient schedules an appointment with a provider or facility and completes his/her patient registration information, as stated by the American Academy of Professional Coders (AAPC). At this juncture, the check-in staff should verify the patient’s insurance eligibility and should collect appropriate patient financial responsibilities such as copayments, past-due balances, and deductibles. Confirming insurance eligibility and collecting patient financial responsibility are critical to the front-end medical billing process so that patient payments are collected in a timely manner without having to send out repeated notices on the back-end, wherein the chance of collections diminishes significantly.
Once the provider sees the patient and signs-off on the patient encounter note, the medical billers and coders will ensure the correct codes are entered in the charge note to create a superbill. As explained by the American Academy of Family Practice (AAFP), the superbill is an itemized form that healthcare entities use to create claims. By utilizing data within a superbill, the medical biller can manually or electronically prepare a claim for submission to payers. Generally, these forms are prepared in various specified formats for different private insurance payers, prepared on the CMS-1500 form for non-facility Medicare submissions, or prepared on the UB-04 for facility Medicare submissions.
Once the claim is prepared in the appropriate format, the medical biller will transmit the claim to a Clearinghouse contracted with the service-rendering provider’s organization. The clearinghouse ensures that the claim has all of the appropriate data and formatting necessary for claim submissions to payers. If an error is found, the claim will be rejected, and the biller will have to resubmit the claim. Once approved, the claim gets transmitted to the payer.
When the payer receives the claim, the settlement process initiates, wherein the payer assesses the claim and makes a decision to accept the claim totally, deny the claim totally, requested additional medical records documentation to support the claim, or provide partial payment of the claim. An Electronic Remittance Advice (ERA) form will be sent by the payer to the rendering provider’s organization detailing what services were paid, what services were denied, and what pieces of additional supporting documentation may be necessary in order for the provider organization to get paid for services rendered. Denial management is a crucial step in the medical billing process. Failure to follow-up on denials in a timely manner can be extremely detrimental for healthcare organizations, resulting in a loss of revenue and dwindling cash flow.
Just as payer reimbursements come through, typically electronically but sometimes by check, and get tracked and posted into a Practice Management System utilized by the healthcare organization, likewise patient payments are tracked and posted. Any outstanding patient payments require timely follow-up by the medical billing Accounts Receivables (AR) team, generally first with soft reminder calls, mailed bills, and ultimately via a collections agency. Just like Denial Management, AR Management is necessitated in order for provider organizations to collect what is owed to them by patients and payers in a timely manner.
What is Medical Coding?
Medical coding intersects with medical billing during the process of creating claims. Medical coding involves analyzing clinical documentation populated by the provider in order to ensure that all diagnoses are properly codified into the Center for Medicare and Medicaid Services’s (CMS’s) International Classification of Diseases, 10th Revision, Clinically Modified (ICD-10-CM) code set and that the services rendered by the provider get appropriately and accurately formatted into the American Medical Association’s (AMA) Current Procedural Terminology (CPT) code set. These codes sets, along with other code sets such as HCPCS procedural codes, Facility codes, Charge capture codes, Professional codes, and Code Modifiers are typically alpha-numerical codes that signify specified clinical information regarding diagnoses ascertained and services rendered by providers. Thus, medical coding involves the analysis of medical records in order to properly populate all clinical data for payment, whereas medical billing involves the use of these rendered codes to create and submit claims to payers and bills to patients.
When a provider discharges a patient from a facility or the patient leaves the provider’s outpatient office, a medical coder is responsible for reviewing clinical documentation in order to generate the appropriate codes for the medical biller to create a claim out of. Ensuring that the codes precisely reflect what the provider documented in his/her patient encounter is crucial so to prevent claims from being denied, curtail and win extensive appeals processes, and reduce the risk of claim audits by CMS.
Conclusion
Medical billing and coding are foundational healthcare revenue cycle management (RCM) processes. The medical billing and coding process initiates with patient registration and only truly terminates when the provider has received payment in full from payers as well as the patient for all services rendered to the patient. Proper management the Revenue Cycle and the medical billing and coding processes is absolutely critical for all healthcare organizations in order to maintain financial viability and continue to offer patient care services.
Is your organization facing medical billing and coding challenges? Contact us for more information on our Revenue Cycle Management services.
